Relationships March 18, 2017


Why would someone elect to have major surgery when it can be avoided and makes no difference in treating the disease?
This is the question some breast surgeons are now asking themselves in light of a troubling new trend in which breast cancer patients are asking to have both of their breasts removed (a bilateral mastectomy), even though one breast is unaffected by the disease.
Removing the healthy breast, which is known in medical speak as contralateral (opposite breast) prophylactic (preventive) mastectomy or CPM, is on the rise and part of a growing debate in the U.S. about overtreatment in medicine. Yet in this case, it’s the patients who are pushing for more aggressive treatments, not the doctors.
For example, research has shown that in 1998 only two percent of patients with Stage 0 to III breast cancer opted for a double mastectomy. By 2011, that number jumped to 12.3 percent. Today, some surgeons think the number is closer to 20 percent.
Even more troubling is the number of younger women opting for the invasive surgery. In 2011, 33 percent of women under 40 chose to remove both breasts. The problem is that a bilateral mastectomy doesn’t increase survival rate any more than a lumpectomy with radiation, and so doctors are puzzled as to why so many women are asking for it.
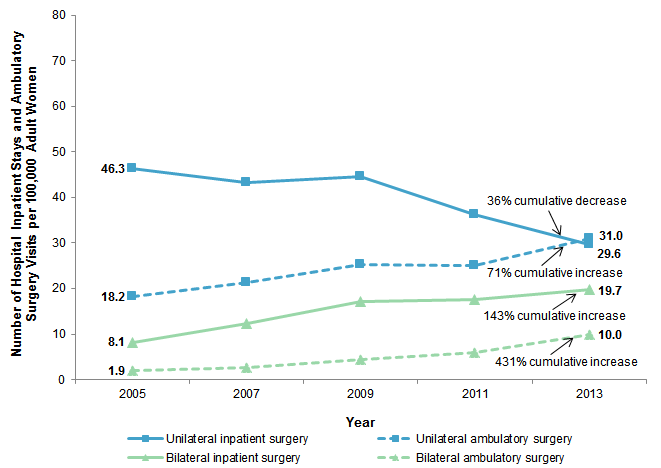
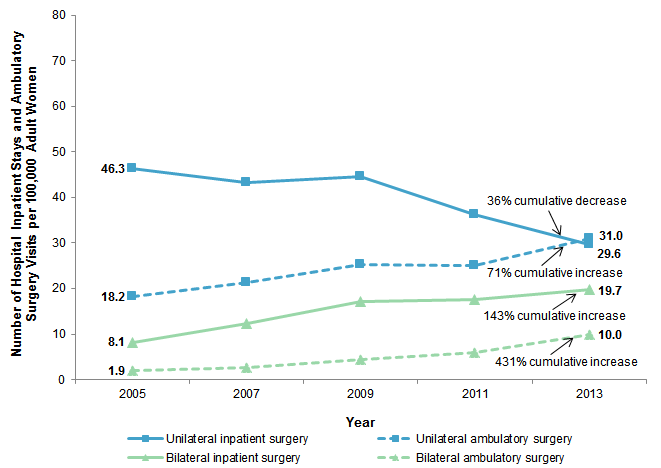
The rise in bilateral mastectomies. Source: Trends in Bilateral and Unilateral Mastectomies in Hospital Inpatient and Ambulatory Settings, 2005-2013 (Feb. 2016)
“I asked about 500 surgeons, ‘How many of you recommend bilateral mastectomy in patients with average risk breast cancer,’” said Steven Katz, a professor of medicine, health management, and policy at the University of Michigan in Ann Arbor. “No one raised their hand,” he told me. “Surgeons are not enthusiastic about this procedure.”
According to a 2016 study from Duke University, not only does opting for a double mastectomy not increase your survival, it doesn’t exactly increase your quality of life either. “You’re not better off, you’re not happier, you don’t feel better about yourself sexually by having the healthy breast removed,” said E. Shelley Hwang, the chief of breast surgery at Duke Cancer Institute, who led the 2016 study.
So what’s going on? We spoke to doctors, oncologists and breast cancer experts to find out why so many patients are asking for an arguably overzealous treatment.
? ? ?
Breast cancer awareness has indeed risen over the years, and the fact that one in eight women will develop breast cancer in their lifetime means more women know women with breast cancer.
This exposure can be positive, but it can also lead women to ask for the same treatment their friend, sister or colleague had based on nothing more than familiarity.
“Patients know other women who have had a [bilateral mastectomy], who feel good about it. So now when a patient is diagnosed, they already have this narrative in the room,” says Katz. And that narrative intensifies when a celebrity, whose treatment choices can reach millions, is involved.
For example, back in May 2015 celebrity chef Sandra Lee announced to the world that she had been diagnosed with breast cancer and would undergo a double mastectomy. In an interview with Good Morning America she said her doctors told her she was a “ticking time bomb” and she chose to have both her breasts removed because she “never wants to go through this again.”
Lee was diagnosed with DCIS, a non-invasive breast cancer — sometimes referred to as Stage 0 — which in many cases will never turn into invasive cancer at all. And she tested negative for any genetic predisposition to breast cancer.
So while her struggle is real, her message is dangerous.
Here’s why: Having a double mastectomy does not mean the cancer will not return and this major misconception about breast cancer and its treatment is part of the problem.
“Bilateral mastectomy reduces the possibility of cancer in the unaffected breast, but it cannot reduce the distant recurrence,” explained Katz, “which overwhelmingly occurs in other parts of the body.”
In other words, the cancer doesn’t usually come back in the healthy breast anyway. If there is a recurrence of cancer it occurs in another part of the body. Which is why having both breasts removed doesn’t improve survival rates.
Mary Hooks, a surgical oncologist at Vanderbilt-Ingram Cancer Center, echoed this sentiment adding, “[Many women] believe the second cancer is metastasized from the first cancer,” which she says “fuels the fire” for a bilateral mastectomy. But in reality that doesn’t happen very often. She explains, “What we see is a second cancer.”
But women aren’t receiving this message. Instead, thanks in part to the media and celebrity endorsement, the message they’re seeing is that removing both breasts will mean the days of cancer are behind them. Hooks says many patients decide on a double mastectomy because they think, “I want them off, I don’t want to have to deal with that again,”she says, noting that it’s fear which drives this psychology.
Celebrity awareness therefore is a “double edged sword”, she says.
“You could not get an appointment with one of our genetic counselors for months after Angelina Jolie,” she explained, referring to Jolie’s very public decision to remove both of her breasts back in 2013. “She rose awareness but it also gave rise to unsound fear.”
This phenomenon has been deemed, “The Angelina Effect” but the problem is — as Hooks points out — most people don’t understand what Jolie did and why she did it.
Jolie discovered she carried a genetic mutation in the BRCA1 and BRCA 2 genes which made her odds of getting breast cancer much, much higher than the rest of the population. (FYI: Of all breast cancer cases only about five to 10 percent have the BRCA mutations. Jolie’s case therefore is rare).
“I think Angelina did the right thing for herself … but I think a lot of people misunderstood it because it’s complex stuff,” says Hooks.
Panic is no doubt the driving force here — and when celebrities refer to early stage breast cancer as a “ticking time bomb”, as Lee did, it reinforces that sense of urgency.
“It’s instilling fear in them,” says Hooks. “Frequently what we see is that women’s first fear is their own mortality.” Which is why experts told me that more accurate information is needed in order to push back against pop-culture mastectomies.
? ? ?
A cancer diagnosis is terrifying and most patients want to feel like they did everything in their power to beat the disease, says Michigan’s Katz.
When women are diagnosed they have three main objectives, he explains: Get home to family. Never come back again. And if something bad does happen they want to feel like they did everything in their power to prevent it.
“If you add those up you get double mastectomy,” Katz says.
Of course “everything in their power” only leads to dramatic treatment thanks to misinformation.
“It’s very hard for women to wrap their heads around the fact that when breast cancer spreads it doesn’t spread to the other breast, it spreads to other parts of the body,” explained Elisa Port, associate professor of surgery at Mount Sinai School of Medicine and author of “The New Generation Breast Cancer Book.”
“Removing the other breast in no way affects your survival. All you’re doing is removing healthy breast tissue.”
Of course there are other reasons for double mastectomy outside of survival as Port, Katz and other experts explained. For instance a lumpectomy, in which doctors only remove the cancerous tumors, can be just as effective in treating the cancer but is done in conjunction with radiation which some women want to avoid.
A unilateral mastectomy (only removing the cancerous breast) is also an option, but for some women having one breast reconstructed and one natural breast feels off balance so they choose a double mastectomy for cosmetic reasons and to avoid the stress of future screenings.
All of these reasons are valid — and all the experts stressed that each treatment decision is up to the individual and should be respected — but at the same time patients need to understand “what they’re getting and what they’re not getting from their treatment” says Port. “That’s the most interesting and intense part of my job.”
What they’re not getting with a double mastectomy is a cancer-free guarantee — and that’s a hard message to sell.
? ? ?
Let’s be clear: A bilateral mastectomy with reconstruction is a major surgery which comes with it’s own set of risks, such as blood loss, infection and risk during anesthesia, which is why surgeons want women to contemplate all treatment options before deciding on the invasive procedure. “There are some women who are very unhappy with their own breasts … and think about it as a boob job,” emphasizes Port. “But it’s not.”
For instance, Sandra Lee was famously re-hospitalized after complications arose from her double mastectomy, which included a nasty infection that in turn required more surgery. The point is, it’s no walk in the park and should not be taken lightly.
So how do we get the message across?
“I think we need to get those women who have chosen the breast conservation route to be as outspoken as possible,” said Vanderbilt’s Hooks. She says there was a time in the 1990s and early 2000s in which there was a big push for breast conservation, but all that has changed and mastectomies are taking over.
Katz in Michigan agreed, “You have a paradox,” he says. “Women want to remove both breasts to feel better about their cancer risk, even though it doesn’t reduce the risk at all.” This, he says, is making surgeons “uncomfortable.”
“We [medical professionals] need to reinforce the notion of take your time,” explains Katz. “[Breast cancer] is not a medical emergency. You have time for a second opinion. There’s no need to rush.”
Women who did undergo a double mastectomy, however, should feel empowered by their decision. “Women who had it should feel good about it, but it can lead the next patient astray a little bit,” says Katz. Instead we should take this as an opportunity to start changing the narrative.
As many experts emphasized, breast cancer is not an emergency. Patients should feel like they have time to take a deep breath and figure out what’s going on before making major decisions. Or opting for surgery because a celebrity did.